Questions and Answers
Written by: Prof. Dr. Semih Halezeroğlu
Lung cancer is one of the most common cancers in our country and worldwide. During diagnosis, patients undergo various tests, including imaging, CT scans, PET-CT, and, if necessary, bronchoscopy or needle biopsy. When the results indicate surgery, many questions arise regarding this procedure from patients and their relatives. Below are the answers to these questions.
In Which Cases Is Lung Cancer Surgery Performed?
The most effective treatment for early-stage lung cancer is the surgical removal of the cancerous lung tissue. Being deemed eligible for surgery in lung cancer is a significant opportunity, as not every lung cancer patient is suitable for surgery. Surgery is only performed when lung cancer is detected in its early stages. Unfortunately, only about 1 in 5 lung cancer patients is operable. Sadly, for approximately 80% of patients, lung cancer is diagnosed in stages 3 and 4, where surgery offers no significant benefit.
Lung cancer surgery can be performed if the following three conditions are met:
-
- The cancer has not spread (metastasized) to other organs. This is determined through diagnostic tests, especially PET-CT scans. Surgery can be performed if cancer is confined to the lung and has not metastasized to other organs such as bones, the brain, adrenal glands, or liver.
Lung cancer has four stages, and surgery is only performed in stages 1 and 2 (and in some stage 3 cases).
- The cancer is completely removable. If the cancer has invaded nearby structures (such as the spine, major blood vessels, aorta, esophagus, or heart), complete removal may not be possible, and surgery is not performed in such cases.
- The patient’s heart and lung functions are sufficient. Pulmonary tests and cardiac evaluations are conducted to determine this. If the patient’s heart and lung functions are adequate, the cancerous lung tissue can be removed.
Types of Lung Cancer Surgeries
With the increasing experience of surgeons and advancements in surgical technology, many surgeries previously performed as open procedures are now conducted using minimally invasive methods. The same applies to lung cancer surgeries.
Open Lung Cancer Surgery
In open surgeries, the area between the ribs on the affected side (right or left lung) is cut open. A surgical instrument called a retractor is used to widen the area, and the operation begins.
Although most lung cancer surgeries are now performed using minimally invasive techniques, some cases (such as large tumors, the need for careful separation from adjacent tissues, or previous lung surgeries) may still require open surgery. This is true for approximately 15% of patients, while 85% can undergo minimally invasive procedures.
It is important to note that as the surgeon’s experience with minimally invasive operations increases, the rate of such surgeries also rises. Conversely, less experience leads to higher rates of open surgery.
Minimally Invasive Lung Cancer Surgery
These surgeries can be performed in several ways.
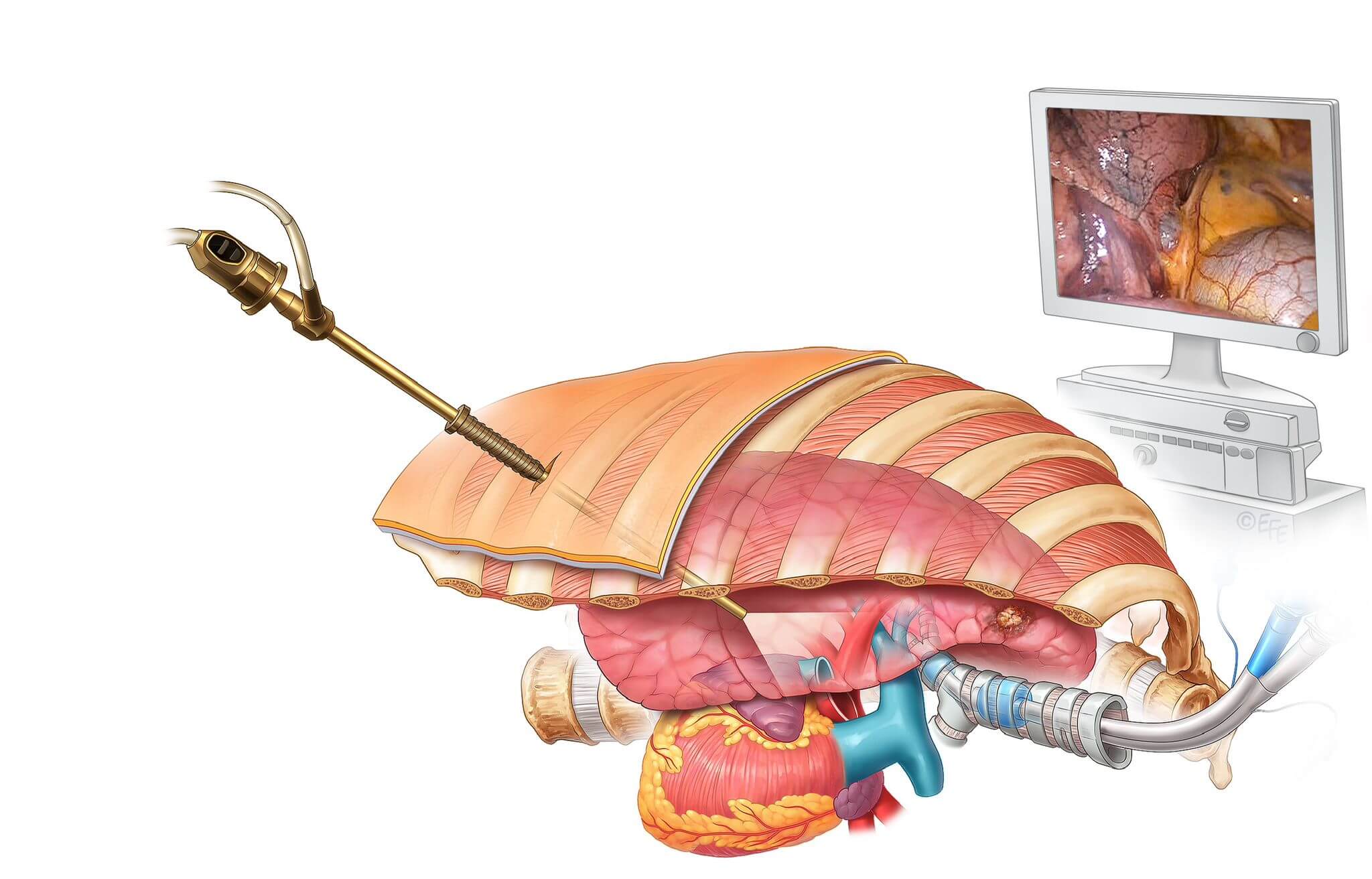
Thoracoscopy is a procedure that allows the examination of the chest cavity using minimally invasive techniques, enabling diagnosis and treatment of lung diseases.
Procedure
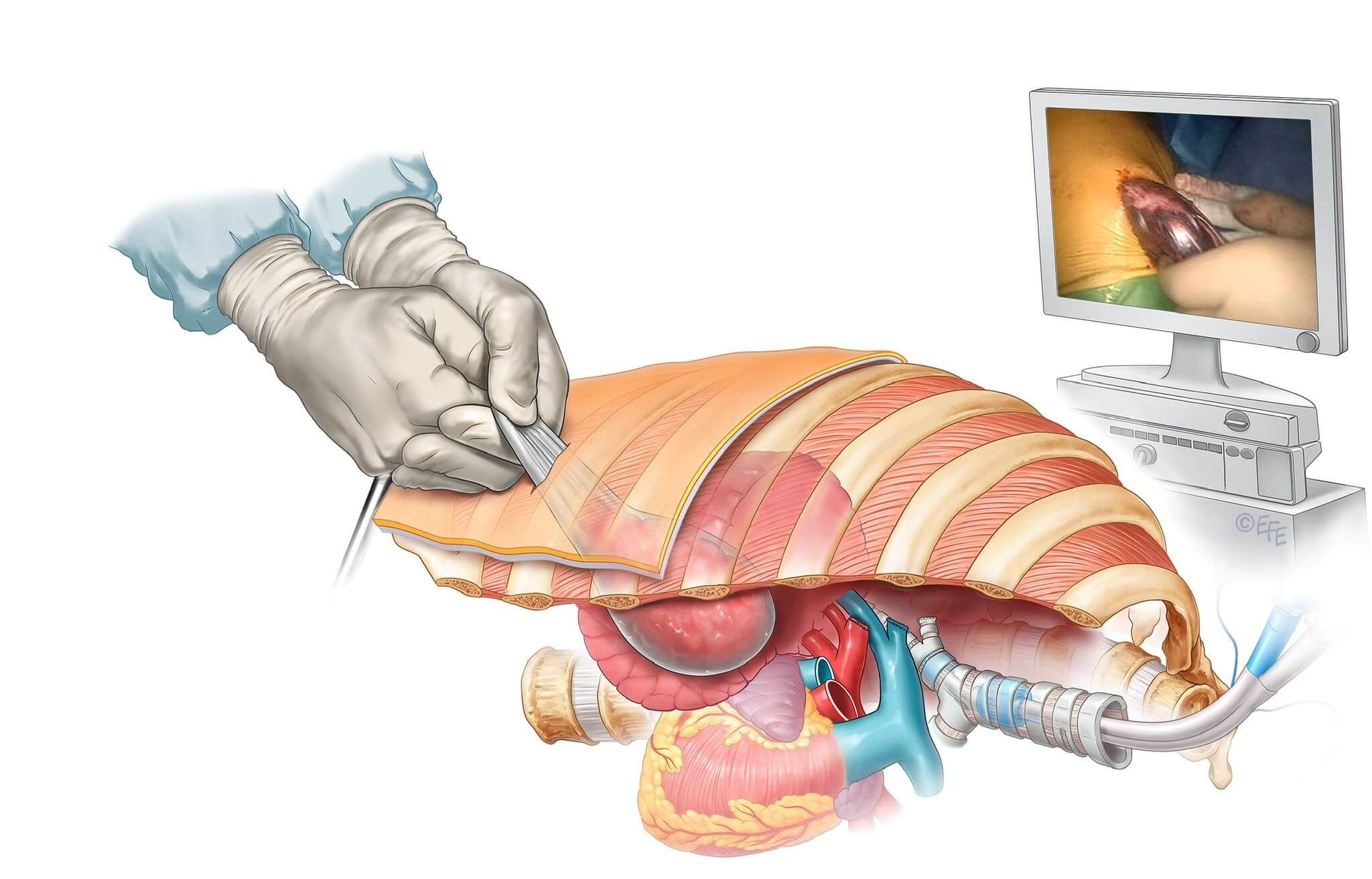
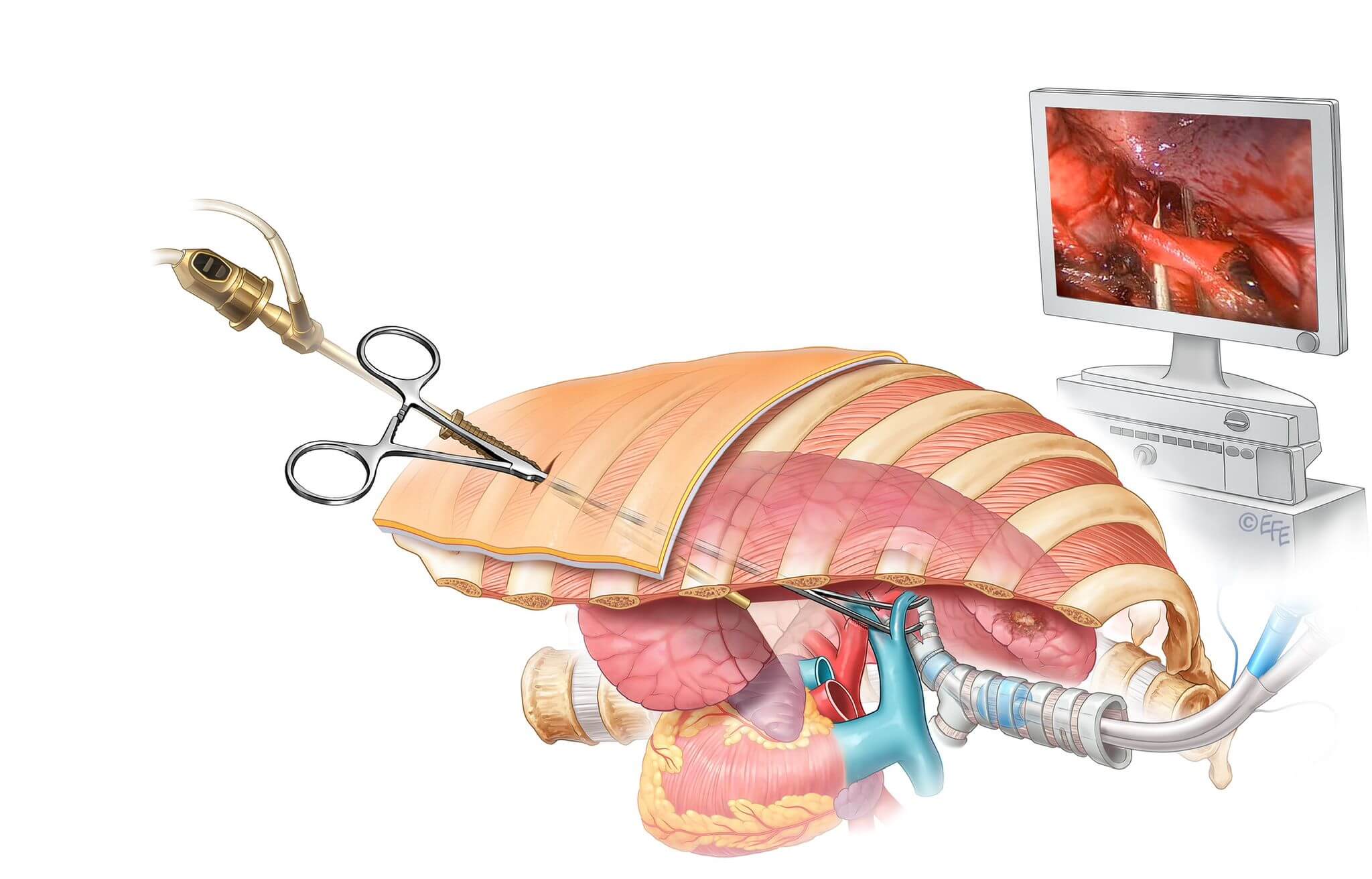
- A small incision is made in the patient’s chest wall during thoracoscopy.
- A thoracoscope (a lighted camera system) and necessary surgical instruments are inserted through this incision.
- The camera projects images of the internal structures onto a screen, allowing the surgeon to work in detail.
- The procedure is typically performed under general anesthesia.
Applications
1. Diagnostic Purposes:
- Biopsy of lung nodules
- Examination of pleural fluid
- Evaluation of anomalies in the lung lining
2. Therapeutic Purposes:
- Lung cancer surgery
- Treatment of pneumothorax
- Removal of mediastinal tumors
- Removal of lung cysts
Advantages
- Minimally Invasive: Less traumatic than open surgery.
- Faster Recovery: Patients are usually discharged a few days after the procedure.
- Less Pain: Smaller incisions result in less postoperative pain.
- Fewer Complications: Reduced risk of infection and bleeding.
Special Technique: Single-Port Thoracoscopy
This technique uses only one incision instead of multiple, making it a less invasive option. It provides significant advantages for patient comfort and recovery time. At our clinic, we perform the Single-Port VATS procedure, prioritizing minimally invasive techniques and patient comfort.
All current international lung cancer treatment guidelines recommend the use of minimally invasive surgery for lung cancer patients.
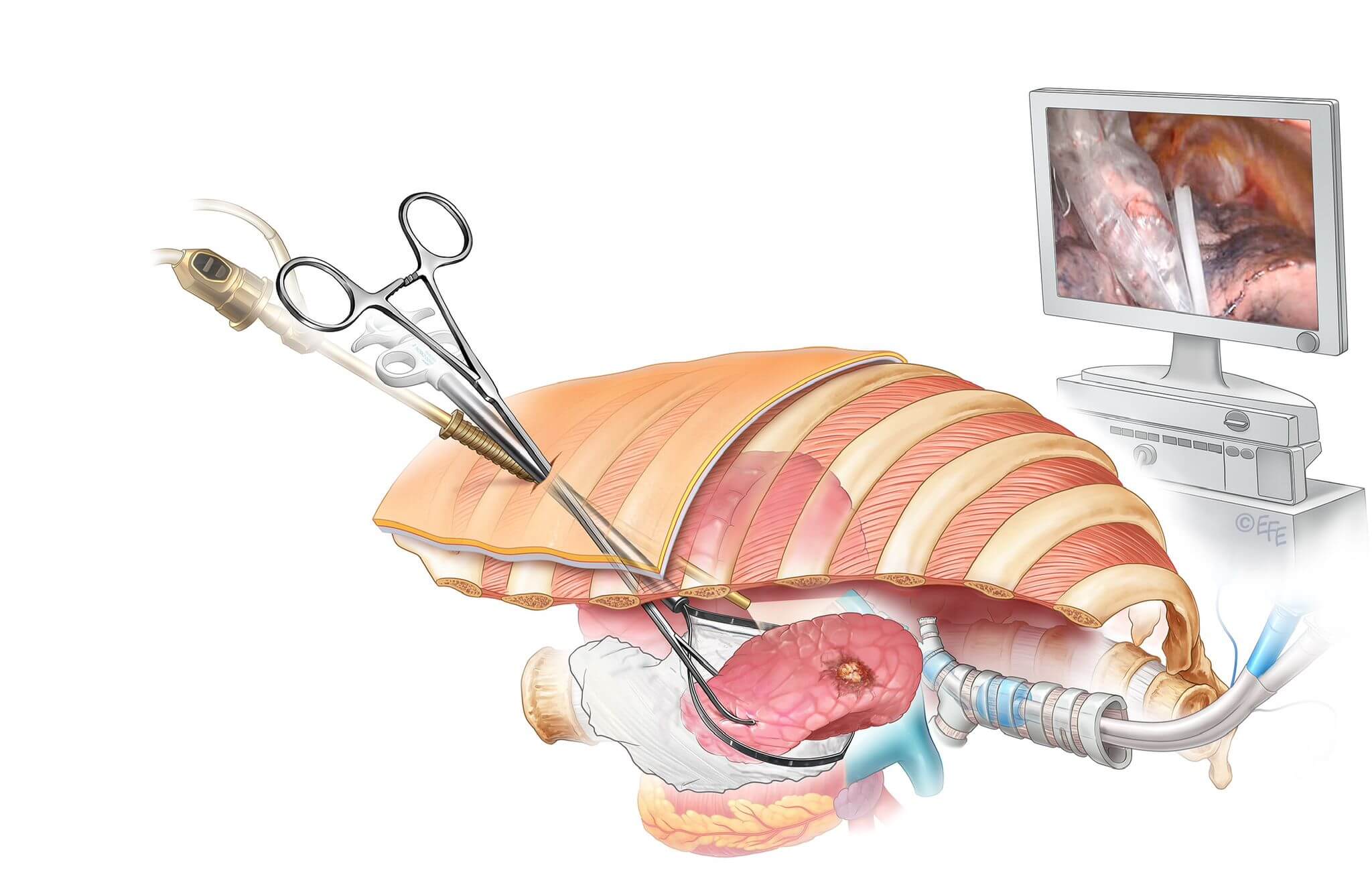
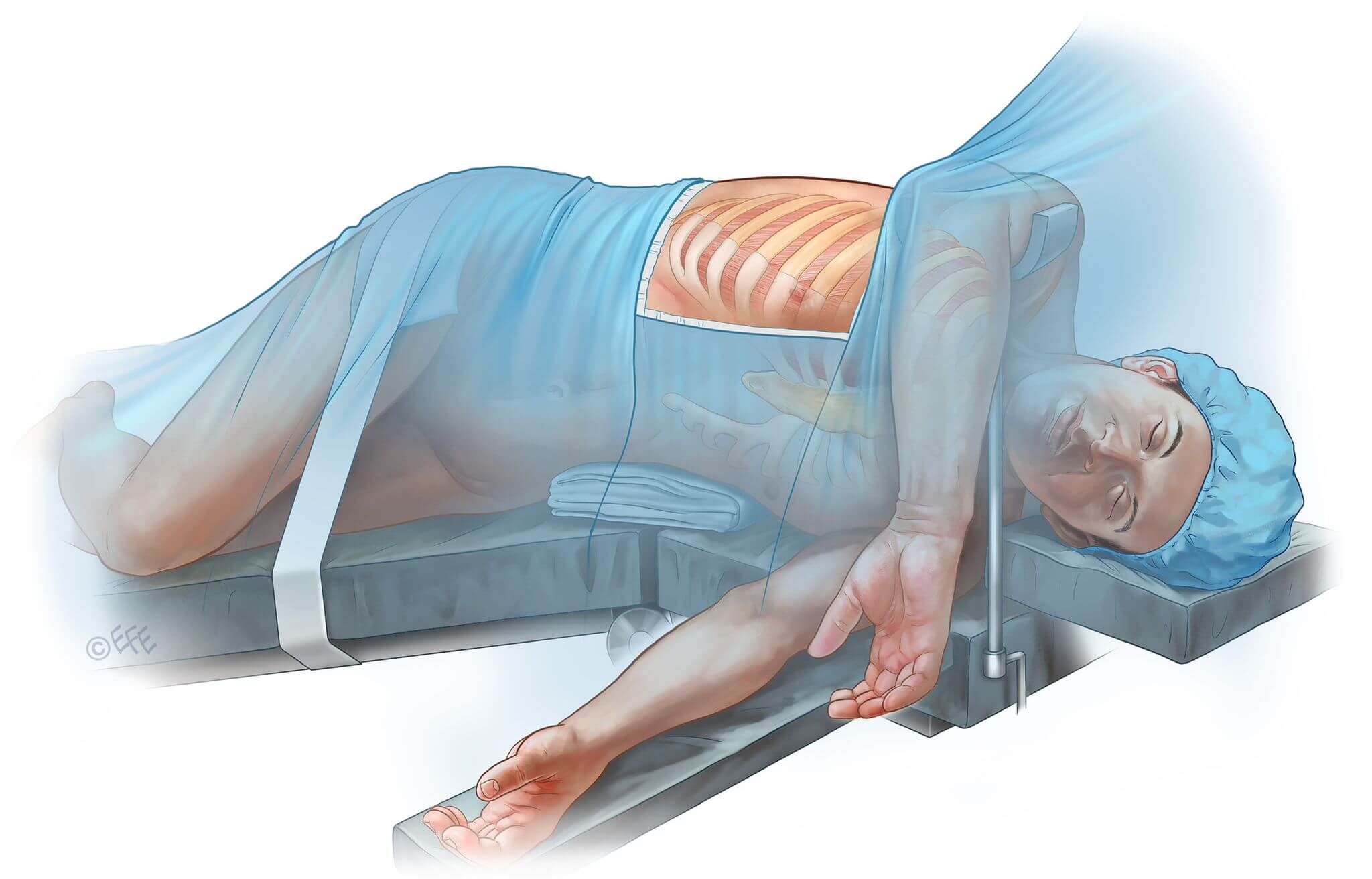
Illustrations of the Surgery
To better explain the procedure, the following illustrations were created by Dr. Levent EFE, one of the leading medical illustrators globally.

The cancerous lung lobe has now been separated from the body. To remove it from the body, this lung segment is placed into a surgical bag (endobag) and carefully extracted from the patient.
How Much of the Lung Is Removed in Lung Cancer Surgeries?
In both open and minimally invasive lung cancer surgeries, not only is the cancerous lung tissue removed, but also at least 10 lymph nodes from 4 different regions are excised. The purpose of removing lymph nodes is to determine whether cancer has spread to these areas. If the pathology examination reveals that there has been a spread, chemotherapy and radiation therapy (radiotherapy) may be necessary after the surgery.
Lobectomy (Removal of One Lobe)
The preferred surgical procedure in lung cancer is the removal of a cancerous lobe (lobectomy). For most patients, the surgery is completed this way. If performed on the right lung, it is referred to as a right upper lobectomy, right middle lobectomy, or right lower lobectomy. If performed on the left lung (which has two lobes), it is called a left upper lobectomy or left lower lobectomy.
Bilobectomy (Removal of Two Lobes Together)
This surgery, which involves the removal of two lung lobes, can only be performed on the right lung. If the upper and middle lobes are removed, it is called an upper bilobectomy; if the middle and lower lobes are removed, it is called a lower bilobectomy. Removing both lobes on the left side is considered a complete lung removal and is referred to as pneumonectomy, which is described below.
Pneumonectomy (Removal of an Entire Lung)
Although the preferred method in lung cancer is to remove only a lobe or lobes, complete removal of the right or left lung (pneumonectomy) may be necessary if the cancer is located on the main airway or a major blood vessel. This procedure is referred to as a right pneumonectomy or left pneumonectomy.
Segmentectomy
In a segmentectomy, a smaller portion (segment) of a lobe is removed. This is typically preferred in patients with restricted lung function, as less lung tissue is removed.
Duration of Lung Cancer Surgery
The duration of a surgery depends closely on the experience of the surgical and anesthesia team performing it. There are significant differences between teams that have been performing a surgery for many years and those who perform it less frequently. Additionally, some lung cancers are larger or located in more challenging areas, or previous lung diseases (such as tuberculosis, pneumonia, or pleurisy) may extend the duration of surgery. Open surgeries also require additional time to open and close the chest cavity, which is not required in minimally invasive procedures. For this reason, open lung surgeries take longer than minimally invasive ones.
When discussing the duration of surgery, it includes not only the time spent performing the procedure but also the anesthesia preparation time. In lung cancer surgeries, anesthesia preparation typically takes 30–45 minutes.
Our team’s average duration for open lung cancer surgeries is 90 minutes, while minimally invasive surgeries take 60 minutes. In summary, the total time from anesthesia preparation to the patient’s recovery ranges between two and two-and-a-half hours.
Chest Tube (Drain)
At the end of the surgery, a chest tube (drain) is placed in the patient. This drain is removed when there is no air leakage in the lung, and the daily fluid output decreases below 250 cc. Removing the drain is not a painful process and typically occurs between the first and fourth postoperative days. In some cases, the drain may need to remain in place for a few additional days if air leakage persists.
The Surgical Team
The surgery is performed by a senior thoracic surgeon, assisted by one or two thoracic surgery specialists and one or two nurses. Additionally, an anesthesiologist and one or two anesthesia technicians are involved.
The success of a surgery heavily depends on the team’s long-term collaboration.
Risks of Lung Cancer Surgery
The risks associated with lung cancer surgery have significantly decreased over the years. However, as with all surgical procedures, risks exist both during and after the surgery. The key is to identify these risks beforehand and take the necessary precautions. For example, patients with insufficient respiratory function or significant heart disease are identified as high-risk candidates before surgery, avoiding unnecessary complications.
In minimally invasive (VATS) lung cancer surgeries, the risks are lower compared to open surgeries.
The following complications occur in approximately 15% of patients:
- Bleeding during surgery
- Postoperative infection
- Respiratory failure
- Brain or heart vessel blockage (embolism)
- Prolonged intensive care treatment
- Chylothorax (lymph fluid leakage into the chest cavity)
- Eyelid drooping
- Hoarseness
- Prolonged drainage
- Pain
- Others
Mortality Risks in Lung Cancer Surgeries
Another critical topic is the mortality rate, i.e., the risk of death during or after surgery. This rate is calculated based on the risk of death within 30 days from the day of surgery. For lobectomy procedures in lung cancer, the 30-day mortality rate ranges between 0.8% and 1.5%. This variation depends on factors such as medical equipment, experience, and the presence of comorbidities (e.g., heart disease, diabetes, or hypertension).
For pneumonectomy, where an entire lung is removed, the 30-day mortality rate is 7% for the right lung and 5% for the left lung. Therefore, in cases where pneumonectomy is planned, patients’ heart and respiratory functions must be examined more comprehensively than those undergoing lobectomy.
Is Postoperative Intensive Care Necessary?
In recent years, the need for intensive care has significantly decreased for patients undergoing lobectomy. In our practice, patients with additional heart conditions or those who have had an entire lung removed are kept in intensive care for one night. Otherwise, normal ward follow-ups are conducted.
How Long Is the Hospital Stay After Surgery?
The average hospital stay after minimally invasive surgeries is 3 to 4 days, while open surgeries require 5 days. If an entire lung is removed, the hospital stay averages 6 days.
When Can Patients Return to Normal Life After Surgery?
Patients who undergo minimally invasive surgery can return to their normal life within one week after discharge. For open surgeries, this period is approximately three weeks.
Is Postoperative Medication (Chemotherapy) or Radiation Therapy Necessary?
Postoperative chemotherapy or radiation therapy is required if the pathology report indicates a tumor larger than 5 cm in diameter or if cancer has spread to the lymph nodes. If the tumor is smaller than 5 cm and there is no lymph node involvement, no further treatment is needed.
In the videos below, you can watch the real-life stories of our patients who underwent surgery for lung cancer.
Video:1 Closed Operation Due to Tumor Presenting with Back Pain
Video 2: Chemotherapy and Radiotherapy First, Then Closed Surgery